
Serena Vukosavic
Serena Vukosavic is completing a Bachelor of Arts degree in Applied Psychology at Capilano University, where she has been named to the dean’s list for academic excellence. During her studies, she completed a practicum with an outdoor learning program, gaining valuable experience supporting children’s social and emotional development in nature-based settings. Serena is passionate about mental health and supporting the well-being of others. In the future, she plans to pursue a masters in either counselling or social work.
In August of 2024 I was diagnosed with Celiac Disease. That day, I was overwhelmed with a sense of relief along with confusion. It took over a year, several tests and misdiagnoses. It was an endless cycle of blood work, ultrasounds and inconclusive doctor appointments. I was constantly going to the doctor and being told everything was fine when I knew I wasn’t. I remember at one of my doctor appointments I had written a lengthy list of symptoms in my notes. My symptoms ranged from abdominal pain to my hands randomly becoming swollen and numb. I insisted something was wrong with my digestive system as my symptoms did not seem normal, however, I was told “everyone has IBS.” It wasn’t until a few months later, when my symptoms and anxiety were becoming unbearable, that I went back to the doctor. That’s when my doctor ordered more blood work which ultimately led to my Celiac diagnosis. I was essentially just told to go on a gluten free diet and that it’s a genetic disease, not being given much information beyond that. However, I quickly learned it was far more complex than just eating gluten free. At the time, I didn’t realize that this wasn’t just a diet change but an autoimmune disease that would affect both my mental and physical wellbeing. After getting diagnosed, I was puzzled because no one in my family has a history of any kind of autoimmune disorder, other than my younger brother. It got me thinking, why is it only my brother and I experiencing this? It can’t purely be genetic, could it? Another thing we share other than an autoimmune disorder is childhood adversity. We grew up in and out of the foster care system, experiencing constant instability and various hardships. I wondered whether experiencing that many stressors during crucial development periods had a negative impact on our health.
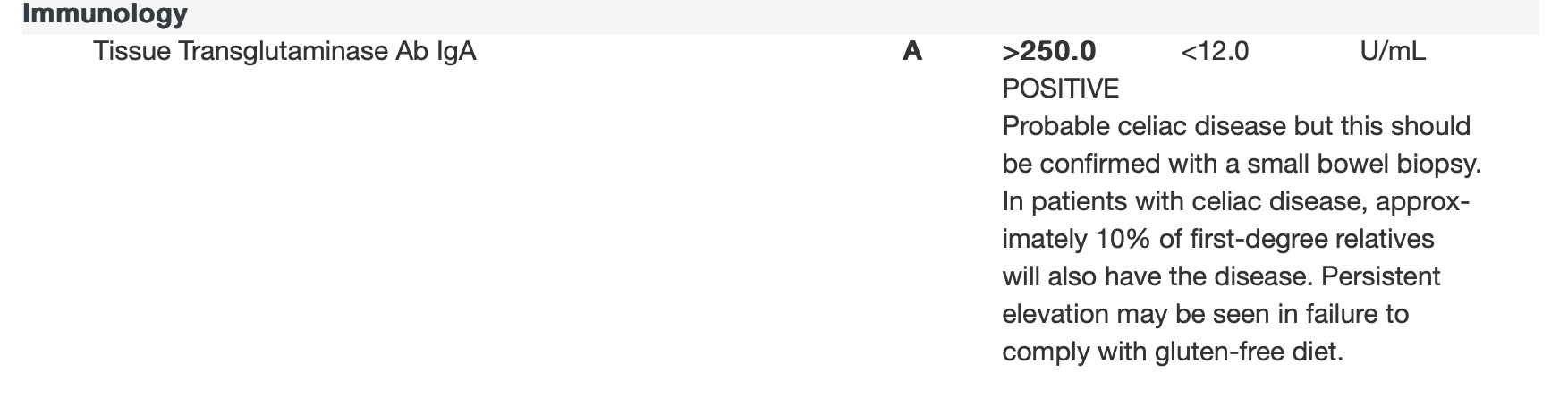
This is a screenshot of my blood test results indicating that I have Celiac Disease.
What are Autoimmune Disorders?
An autoimmune disorder is when the immune system is overactive, and the body attacks itself (Cleveland Clinic, 2025). Our immune systems fight off invaders like viruses or bacteria however, someone with immune dysfunction, the body mistakenly attacks healthy tissue (Cleveland Clinic, 2025). These conditions are chronic and require lifelong management (Cleveland Clinic, 2025). There are over 100 different kinds of disorders, affecting any part of the body such as joints, muscles, skin, blood vessels, digestive system, endocrine system and nervous system (Cleveland Clinic, 2025). Some of the most common types are Lupus, Rheumatoid arthritis, Psoriasis, Crohn’s disease, Celiac disease, Type 1 Diabetes, Hashimoto’s Thyroiditis, Graves’ disease and Multiple Sclerosis (Cleveland Clinic, 2025). These are diagnosed through physical exams, blood tests, family history, ultrasounds, x-rays, magnetic resonance imaging and computed tomography (Cleveland Clinic, 2025).
Treatments will vary based on what autoimmune disorder one has and is personalized to fit an individual’s needs (Cleveland Clinic, 2025). Treatments consist of pain relievers, IVIG infusions, occupational therapy, anti-inflammatory medication, immunosuppressants, physical therapy, adherence to a gluten free diet and insulin therapy (Cleveland Clinic, 2025). Due to the fact the causes surrounding the development of these conditions are generally unknown, it is difficult to determine prevention methods (Cleveland Clinic, 2025). Additionally, individuals with existing autoimmune disorders are at an increased risk of developing more (Global Autoimmune Institute, n.d.). The cause of this is undetermined although genetics along with environmental factors appear to be significant (Global Autoimmune Institute, n.d.).
The Evolution of Autoimmunity
Allergies were the first clear evidence that showed the immune system could attack the body (Ahsan, 2022). During the 1940s, autoantibodies were identified becoming key diagnostic features for diagnosing Lupus and Rheumatoid Arthritis (Ahsan, 2022). However, it wasn’t until the 1950s when autoimmunity began to be accepted, due to clinical studies on chronic thyroiditis (Ahsan, 2022). Then a groundbreaking theory in 1962 was introduced by Frank Macfarlane Burnet and Ian Mackay: the immune system has the ability to attack healthy body tissue, resulting in autoimmune disorders (WEHI, 2023). This was an idea that seemed absurd, and scientists struggled to accept this theory (WEHI, 2023). Mackay explains how Paul Ehrlich had considered the concept of autoimmunity in the early 1900s, but it was dismissed as being impossible (WEHI, 2023). This was just the beginning of reoccurring patterns of dismissal in this area of health.
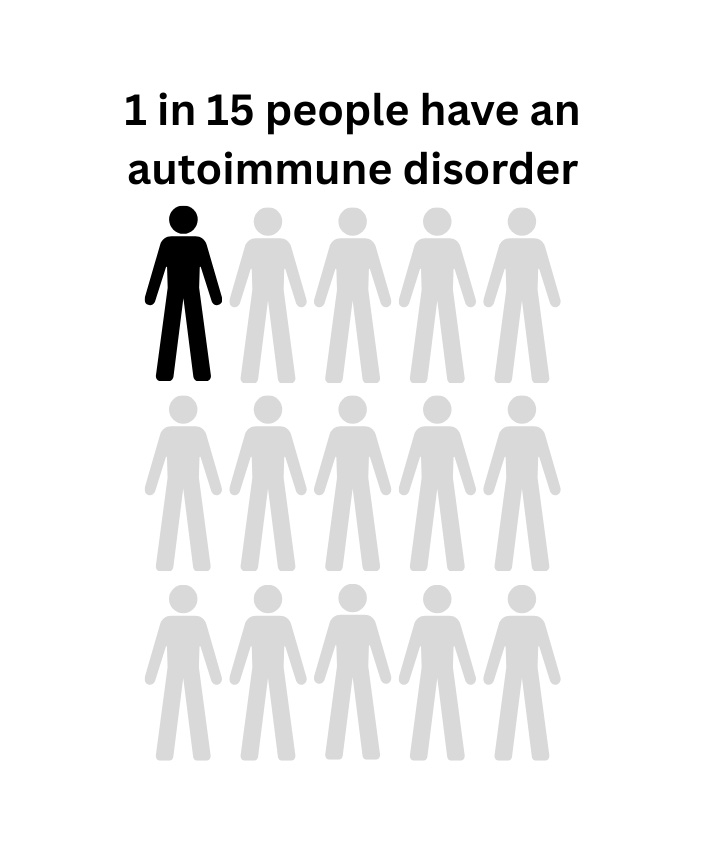
Autoimmune disorders affect one in fifteen people (Cleveland Clinic, 2025). It is a lot more common than people think.
Stress and Immune Function
Psychoneuroimmunology (PNI) is a field that has evolved over the last fifty years (Ader, 2000). This field investigates the interactions between behaviour, neural, endocrine and immune functions (Ader, 2000). Despite the growing, evidence it seems as though it still remains unacknowledged. Exposure to adversity is a strong predictor in relation to immune dysfunction (Kautz, 2021). Kautz (2021), emphasizes that with rising rates of childhood adversity, PNI research must go beyond theory and applied practically. Another study states that 64% of participants with an autoimmune disorder experienced at least one ACE (Dube et al., 2009). Autoimmune disorders affect approximately one in fifteen people in the US (Cleveland Clinic, 2025) and 80% of autoimmune diagnosis are women patients (Goulmamine, Chew & Aninye, 2024). However, historically women are underrepresented in clinical studies (Goulmamine, Chew & Aninye, 2024). I’ve personally encountered barriers of not being taken seriously and symptoms being dismissed as hormonal. This contributes to the current gaps in healthcare, resulting in delays in diagnosis and inadequate treatment. Overall, there is unexplored connection between childhood adversity and autoimmune disorders, and the ongoing dismissal of these conditions is resulting in adequate care.
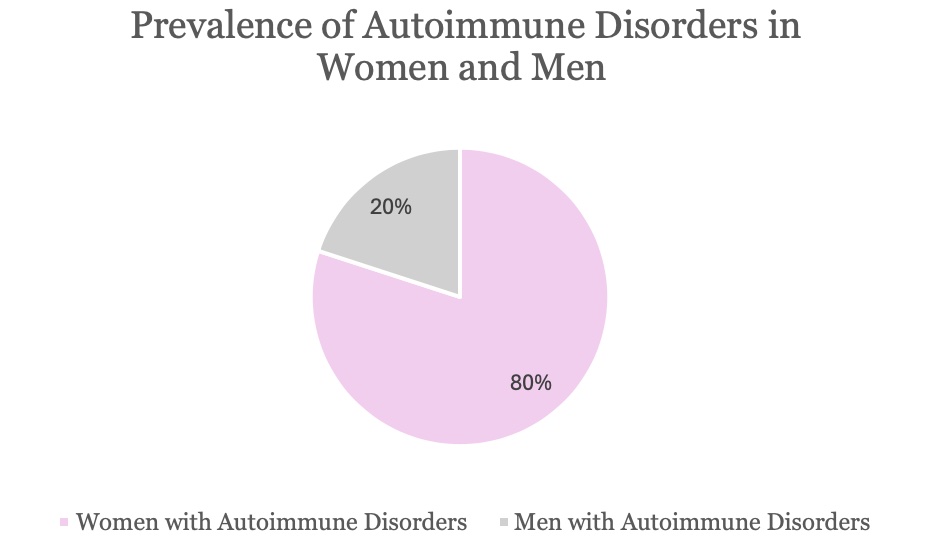
Autoimmune disorders disproportionately affect women (Goulmamine, Chew & Aninye, 2024). Yet the reasons why are not fully understood.
Groundbreaking Studies
In 1975 Ader and Cohen conducted a study in which they discovered that the immune system could be conditioned by associating (taste) with an immunosuppressive drug (Ader & Cohen, 1975). This suggests that the immune system can be suppressed through learned associations (Ader & Cohen, 1975). Ader & Cohen (1975) further explained that it is also not merely due to stress related hormone changes but rather a learned conditioned response (Ader & Cohen, 1975). This was the first foundational study to make this connection.
Kiecolt-Glaser et al., (1987), emphasizes that the impact of chronic stress on the immune system is understudied. In this study blood samples of caregivers versus others that matched socio-demographically (Kiecolt-Glaser et al., 1987). Researchers discovered that those experiencing chronic stress did not show adaptation to stress (Kiecolt-Glaser et al., 1987). The results also showed that caregivers had low levels of T lymphocytes and higher levels of antibodies (Kiecolt-Glaser et al., 1987).
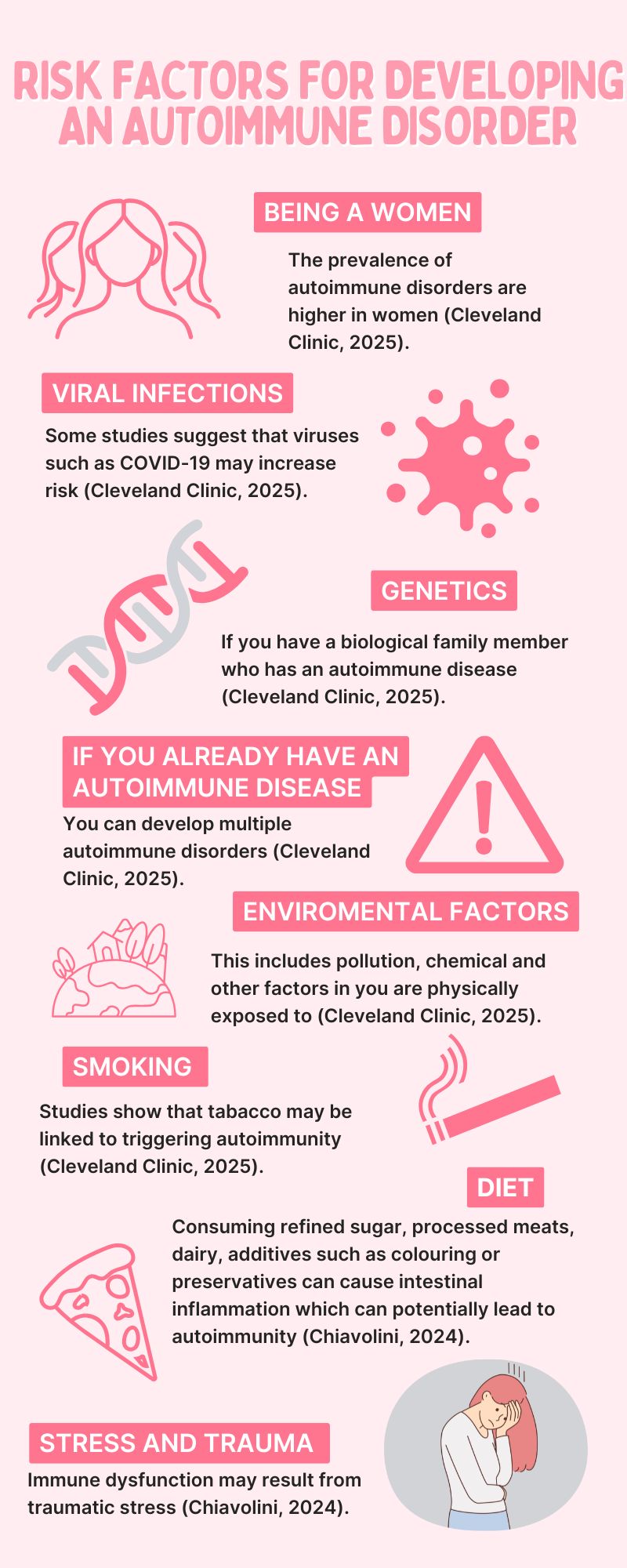
Risk factor infographic created by Serena Vukosavic.
The Present Day
The primary public funder for biomedical research is the National Insitute of Health (NIH) (Act For NIH, 2024). The National Academies of Sciences, Engineering, and Medicine (2022), highlights funding trends indicating that autoimmune research received 1,083,000,000 in funding in 2020. This reflects an increase of 2.6 percent from the previous year (National Academies of Sciences, Engineering, and Medicine, 2022). However, from 2008 to 2020 the NIH has consistently only spent 2.8% of it’s total budget on autoimmune research with no significant increase (National Academies of Sciences, Engineering, and Medicine, 2022). Between 2015 to 2020, the NHI overall funding budget had a 40% increase, meanwhile autoimmune research funding only rose by 34% (National Academies of Sciences, Engineering, and Medicine, 2022). The highest funding was seen in 2020, showing funding is inconsistent (National Academies of Sciences, Engineering, and Medicine, 2022). This demonstrates how autoimmunity research is underfunded and not prioritized in the biomedical field. Even though research has increased regarding potential causes, a lot of studies are recent, and the results are inconsistent. For example, Polick et al., (2022) conducted a comprehensive review of studies looking at childhood adversity and multiple sclerosis. Ten out of the twelve studies suggested a connection between adversity and multiple sclerosis (Polick et al., 2022).
Meanwhile other studies like Macarenco et al., (2022) where they completed a meta-analysis their results indicate that the connection childhood adversity and autoimmune dysfunction is not significant. Another more recent study concluded that the more adversity an individual experiences it increases their likelihood of autoimmune dysfunction (Köhler-Forsberg et al., 2025). The connection appears to be stronger with certain types such as Sjögren’s, Rheumatoid Arthritis, Polymyalgia Rheumatica, Lupus, and Thyroid Disease (Köhler-Forsberg et al., 2025). In addition, certain types of adversity have higher prevalence like neglect and sexual abuse (Köhler-Forsberg et al., 2025). While this area is still burgeoning, these inconsistencies likely are not due to lack of connection but rather significant barriers including gaps in research.
Addressing the Lack Research
Regensteiner et al., (2025) explains how many diseases can affect women differently, but historically the research and evidence that diagnosing and treatments are based off are from studies done on men. These conditions require a deep understanding of the interactions between environmental factors and genetics to develop effective treatments for everyone (SWHR, 2023). Also, there is an underrepresentation regrading race, ethnicity and those pregnant and lactating (SWHR, 2023). This further limits understanding even more and treatments won’t be affective and applicable with all populations, which impacts treatment outcomes (SWHR, 2023). The Society for Women’s Health Research emphasizes that although there has been progress, there are still significant gaps (SWHR, 2023). Barriers to participate in trials must be removed, more awareness brought to how important it is to participate, not unfairly excluding others, establishing accountability measures and enhance recruitment and make sure they stay involved (SWHR, 2023).
Lived Experience Interview with Orlanda
I connected with Orlanda South, a twenty-two-year-old psychology student. She was diagnosed with Crohn’s disease when she was around sixteen or seventeen years old. She explains how her mom was the first to notice her symptoms. “I feel like with a lot of autoimmune diseases, the first symptoms you’re not the one who recognizes them until someone else is like, why are you doing this” (Orlanda South, personal communication, February 28, 2025). Orlanda recalls her experience while seeking answers for her health concerns, saying, “I felt like I was a bit of a hamster. He tried a bunch of different medications on me.” She describes how her doctor would be too enthusiastic about her issues and was constantly recommending more medication. Orlanda explains how getting diagnosed was a difficult and exhausting process. “I was on a waitlist for a long time to see a stomach specialist. Then finally when I turned 18, I could see a real adult doctor but unfortunately, it was around the start of COVID. I had all my appointments on the phone, and he was so similar to the other doctor, I felt like he didn’t understand the severity of what I was experiencing.” She further explains the rollercoaster of getting diagnosed. “At first, they didn’t want to do a colonoscopy. They were just like oh you have irritable bowel syndrome. I just lived my life of these anti-inflammatory pills for a while, and it really wasn’t helping. So then when we went back my mom was like you need to take her seriously.” This highlights how autoimmune symptoms are often dismissed by doctors. It took her mother to step in for the doctor to finally do a colonoscopy which is what resulted in her diagnosis of Crohn’s Disease.
However, this did not stop here, when she changed doctors, the new one completely dismissed her previous diagnosis and claimed she just had IBS, changing all her medications back. “Then when I finally went to a different doctor, he was let’s do another colonoscopy. And he was like, yeah, you definitely have Crohn’s disease,” she says with frustration. Orlanda explains how her current doctor has been much better. “He switched me onto an infusion medication, so I go into a special clinic every two months and they give me an IV and a drip.” However, it is not working as efficiently as it had been initially, and she has recently been having stomach issues. Orlanda emphasizes how frustrating it can be having an autoimmune disorder and seeking adequate care stating, “Doctors don’t want to see you until you have a severe issue.” She recalls how it has been difficult to book an appointment and how they always connect her with the nurse first. “By the time my appointment comes around I am probably going to feel better. They just seem badly organized, and I’m like, guys, I just don’t want to feel sick anymore,” she says. Additionally, Orlanda does not have any family members with Crohn’s Disease. However, when asked about adversity or stress having an impact, she recalls what she went through the year she was diagnosed. “The year that I was experiencing really bad symptoms was also a year that I was really depressed, I wasn’t going to school or anything. I got transferred from mainstream school to alternative school. I think it was a year into alternative school that I was diagnosed with Crohn’s disease.” She explains how her symptoms worsen during stressful periods and how traveling stresses her out. Her energy levels are significantly impacted, and eating is difficult. “There’s more to it, it affects things like mental health and my ability to do activities. I feel like it’s hard, like function as every other human does.” One final note she makes is that “I don’t know how the doctors can make more time, but it would be nice to be able to have more regular checkups.” Unfortunately, Orlanda’s story is not unusual, I can be confirmed through my own lived experiences and what I have heard and witnessed from others. This is the average experience an individual has when navigating the health care system with an autoimmune disorder.
Quote from my interview with Orlanda.
Conclusion
Psychoneuroimmunology has identified a connection between the immune system and brain (Bower et al., 2019). In the past scientists believed these systems worked independently (Bower et al., 2019). However, evidence from this field suggests that psychological states have an impact on immune function (Bower et al., 2019). Although this connection is established it is not being acknowledged in practical settings (Kautz, 2021). It’s generally unexplored compared to other fields and gaps in research and health care persist. More testing should be done regarding adverse childhood experiences and the treatment toward those with autoimmune disorders must improve. This area needs work. A common pattern I’ve experienced as well as Orlanda is doctors waiting until the symptoms are terrible, which evitability leads to further complications. It is important that autoimmune conditions be taken seriously as the long-term impacts individuals are experiencing only exacerbate their conditions. Autoimmune diseases rank in the top ten causes of death for women under sixty-five (Walsh & Rau, 2011). This statistic serves as a call to action, we must increase research funding and ensure better treatment for women and marginalized groups in health care settings. Greater awareness and incorporating emerging concepts into healthcare settings will foster a more supportive environment and facilitate better outcomes for those suffering from autoimmune conditions.
References
Ader, R. (2000). On the development of psychoneuroimmunology. European Journal of Pharmacology, 405(1–3), 167–176. https://doi.org/10.1016/s0014-2999(00)00550-1
Ader, R., & Cohen, N. (1975). Behaviorally conditioned immunosuppression. Psychosomatic Medicine, 37(4), 333–340. https://doi.org/10.1097/00006842-197507000-00007
Ahsan, H. (2022). Origins and history of autoimmunity—A brief review. Rheumatology & Autoimmunity, 3(1), 9–14. https://doi.org/10.1002/rai2.12049
Bower, J. E., Kuhlman, K. R., Haydon, M. D., Boyle, C. C., & Radin, A. (2019). Cultivating a healthy neuro-immune network: A health psychology approach. Social and personality psychology compass, 13(9), e12498. https://doi.org/10.1111/spc3.12498
Chiavolini, D. (2024, July 29). Beyond genes and smoking: 5 more triggers that heighten autoimmune disease risk ” Global autoimmune institute. Global Autoimmune Institute “. https://www.autoimmuneinstitute.org/articles/beyond-genes-and-smoking-5-more-triggers-that-heighten-autoimmune-disease-risk/
Dube, S. R., Fairweather, D., Pearson, W. S., Felitti, V. J., Anda, R. F., & Croft, J. B. (2009). Cumulative childhood stress and autoimmune diseases in adults. Psychosomatic medicine, 71(2), 243–250. https://doi.org/10.1097/PSY.0b013e3181907888
Global Autoimmune Institute. (2024, July 29). Beyond genes and smoking: 5 more triggers that heighten autoimmune disease risk ” Global autoimmune institute. Global Autoimmune Institute “. https://www.autoimmuneinstitute.org/articles/beyond-genes-and-smoking-5-more-triggers-that-heighten-autoimmune-disease-risk/
Global Autoimmune Institute. (n.d.). Risk factors: Global autoimmune institute. https://www.autoimmuneinstitute.org/7-ad-risk-factors/
Goulmamine, S., Chew, S., & Aninye, I. O. (2024). Autoimmune Health Crisis: An Inclusive Approach to Addressing Disparities in Women in the United States. International journal of environmental research and public health, 21(10), 1339. https://doi.org/10.3390/ijerph21101339
Kautz M. M. (2021). Applications of psychoneuroimmunology models of toxic stress in prevention and intervention efforts across early development. Brain, behavior, & immunity – health, 16, 100322. https://doi.org/10.1016/j.bbih.2021.100322
Kiecolt-Glaser, J. K., Glaser, R., Shuttleworth, E. C., Dyer, C. S., Ogrocki, P., & Speicher, C. E. (1987). Chronic stress and immunity in family caregivers of Alzheimer’s disease victims. Psychosomatic Medicine, 49(5), 523–535. https://doi.org/10.1097/00006842-198709000-00008
Köhler-Forsberg, O., Ge, F., Aspelund, T., Wang, Y., Fang, F., Tomasson, G., Thordadottir, E., Hauksdóttir, A., Song, H., & Valdimarsdottir, U. A. (2025). Adverse childhood experiences, mental distress, and autoimmune disease in adult women: findings from two large cohort studies. Psychological medicine, 55, e36. https://doi.org/10.1017/S0033291724003544
Macarenco, M.-M., Opariuc-Dan, C., & Nedelcea, C. (2022). Adverse childhood experiences, risk factors in the onset of autoimmune diseases in adults: A meta-analysis. Professional Psychology: Research and Practice, 53(1), 69–79. https://doi.org/10.1037/pro0000430
National Academies of Sciences, Engineering, and Medicine; Health and Medicine Division; Board on Population Health and Public Health Practice; Committee for the Assessment of NIH Research on Autoimmune Diseases. Enhancing NIH Research on Autoimmune Disease. Washington (DC): National Academies Press (US); 2022 Jun 2. 6, Analysis of Institute and Center Autoimmune Disease Research Activity. Available from: https://www.ncbi.nlm.nih.gov/books/NBK605866/
Polick, C. S., Polick, S. R., & Stoddard, S. A. (2022). Relationships between childhood trauma and multiple sclerosis: A systematic review. Journal of Psychosomatic Research, 160, 1–11. https://doi.org/10.1016/j.jpsychores.2022.110981
Regensteiner, J. G., McNeil, M., Faubion, S. S., Bairey-Merz, C. N., Gulati, M., Joffe, H., Redberg, R. F., Rosen, S. E., Reusch, J. EB., & Klein, W. (2025). Barriers and solutions in women’s Health Research and Clinical Care: A Call to Action. The Lancet Regional Health – Americas, 44, 101037. https://doi.org/10.1016/j.lana.2025.101037
Society for Women’s Health Research. (2023, March). https://swhr.org/wp-content/uploads/2023/03/SWHRFederalResearchBrief2023.pdf
Cleveland Clinic. (2025, February 8). What are autoimmune diseases?. https://my.clevelandclinic.org/health/diseases/21624-autoimmune-diseases
WEHI. (2023, July 28). WEHI history: 1962 Mackay and Burnet’s autoimmunity theory. https://www.wehi.edu.au/about/history/autoimmunity-theory/
Act For NIH. (2024, November 1). 10 things you need to know about the NIH https://www.actfornih.org/10-things-you-need-to-know-about-the-n/
National Institutes of Health, Office of Research on Women’s Health. (2024). NIH-Wide Strategic Plan for Research on the Health of Women 2024–2028. https://orwh.od.nih.gov/sites/orwh/files/docs/ORWH_NIH-Wide%20Strategic%20Plan_FY2024-2028-508C.pdf
Walsh, S. J., & Rau, L. M. (2011). Autoimmune diseases: a leading cause of death among young and middle-aged women in the United States. American Journal of Public Health. https://ajph.aphapublications.org/doi/pdf/10.2105/AJPH.90.9.1463
