
Emma Gerke
Emma A. Gerke (she/her) is completing her Bachelor’s of Arts Degree in Psychology at Capilano University. After earning her bachelor’s degree, she plans to pursue a Master’s of Public Health. Presently, she volunteers at the learning centre at the Carnegie Community Centre on the Downtown Eastside.
Eating disorders are a categorization of mental disorders marked by a disturbance in eating behaviors, and are often associated with distressing thoughts and emotions. The three most common eating disorders found in humans worldwide are anorexia nervosa, bulimia nervosa, and binge eating disorder (Feng, et al., 2023). Anorexia nervosa is an eating disorder characterized by a restriction of the amount or type of a food that an individual consumes (Mayo Clinic, 2024). Bulimia nervosa is an eating disorder in which periods of binge eating are followed by bouts of purging, such as self-induced vomiting, laxative use, or prolonged restriction (Feng, et al., 2023). Binge eating disorder involves recurrent binge eating episodes in which an individual consumes a large amount of food within a short period of time (Hilbert, 2023) without being followed by purging behaviors (Rittenhouse, 2021).
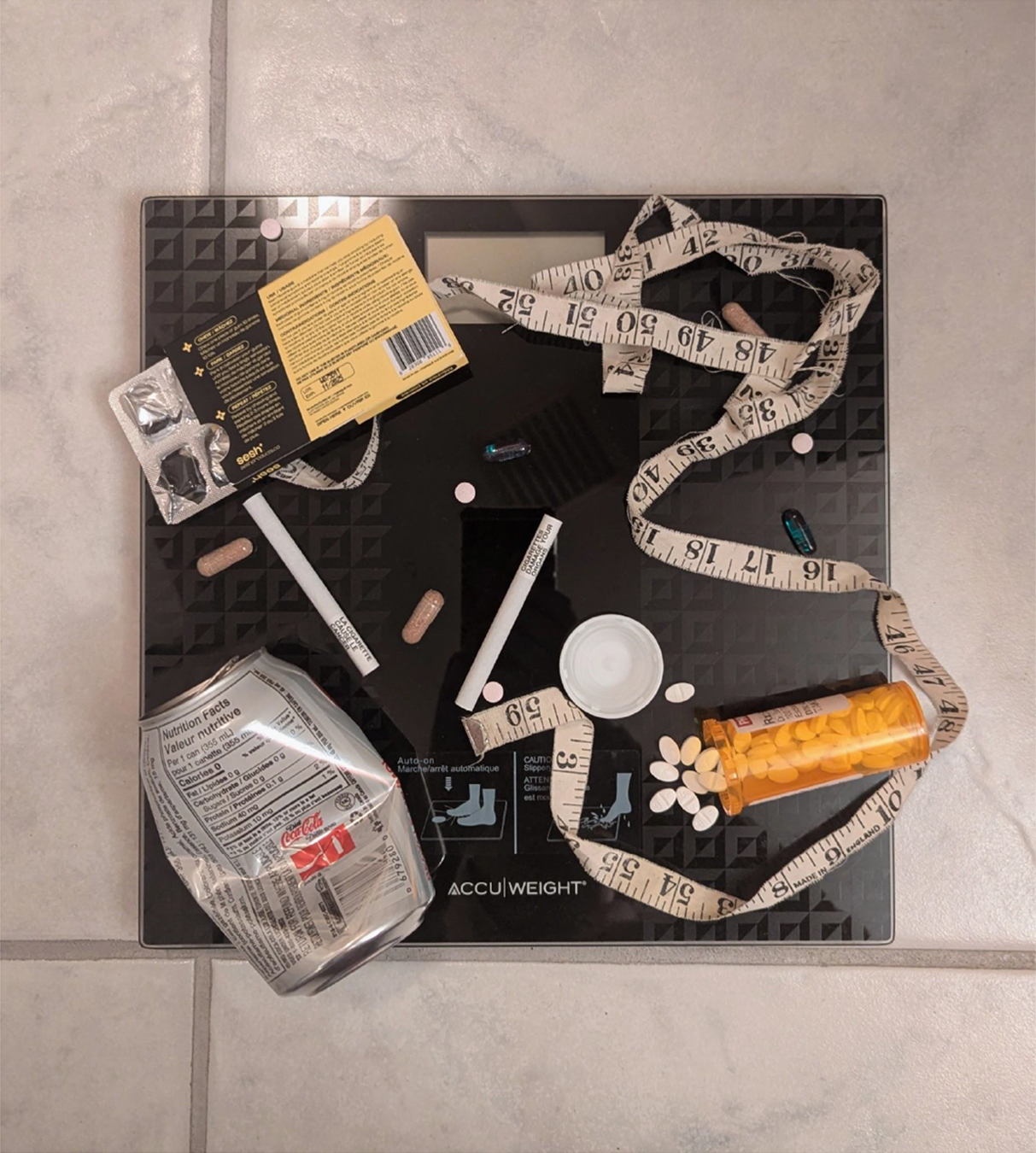
Figure 1. Common symptoms in the three most common eating disorders.
Note. Information within this chart is sourced from Feng, et al. (2023).
Substance use disorder is a mental disorder characterized by an individual’s inability to control their use of substances, including drugs, alcohol, or medications, with the most severe type of substance use disorder being addiction. People diagnosed may also suffer from other mental health disorders, including anxiety disorders, depression (National Institute of Mental Health, n.d.), and eating disorders; with “approximately 50% of individuals with an eating disorder [abusing or being] dependent on alcohol or illicit substances compared with approximately 9% of the general population” (Root, et al., 2011). It has been found that approximately 27% of individuals diagnosed with anorexia nervosa and 23.3% of individuals with binge eating disorder have also been diagnosed with a substance abuse disorder, and bulimia nervosa is the eating disorder believed to be the most prevalent in terms of comorbidity, with 36.8% of individuals with bulimia nervosa having a dual diagnosis with substance use disorder (Rittenhouse, 2021). Although a co-occurrence between eating disorders and substance use has been established, the prevalence varies across studies (Root, et al., 2011). The purpose of this article is to analyze the current existing research, possible theories as to why this comorbidity exists, and to look into the future of research on this topic.
Analysis of Existing Research on Substance Use and Eating Disorders
Research has found that individuals with eating disorders often have a high level of alcohol and drug usage, often meeting the criteria for a substance use disorder (Wolf & Maisto, 2000). In general, a comorbidity with alcohol use disorders (AUD) occurs more frequently than a comorbidity with illicit drug use disorders (IDUD) for eating disorders (Bahji, et al., 2019). A majority of the existing research on the comorbidity or eating disorders and substance use disorders focuses on young women. This is likely due to the fact that a majority of cases of eating disorder are diagnosed during adolescence, and eating disorders primarily affect women, with only 10% of eating disorder cases being men. According to The National Center on Addiction and Substance Abuse, approximately 50% of women who have an eating disorder have substance use disorder, and similarly, the rates of eating disorders are high among those with substance use disorder (Eskander, Chakrapani, & Ghani, 2020).
Eating Disorder Types and Comorbidities
As previously mentioned, the three most common types of eating disorders are anorexia nervosa (AN), bulimia nervosa (BN), and binge eating disorder (BED) (Feng, et al., 2023). Within anorexia nervosa exists further subtypes; anorexia nervosa subtype restricting (AN-R) is characterized by long periods of fasting, dieting, and excessive physical activity, and anorexia nervosa subtype binge/purge (AN-B/P) is marked by recurrent episodes of binging, followed by episodes of compensatory behaviors known as purging, which can include the use of laxatives, self-induced vomiting, or excessive exercise in order to regain a sense of control (Easton, 2023).

Figure 2. Common symptoms of the anorexia nervosa subtypes
Note. information within this chart is sourced from Easton (2023).
Although both AN-BP and BN are characterized by episodes of binging followed by purging, the key difference between these disorders is that individuals with AN “… have significantly low body weights for age and height, [which is] considered an important difference, diagnostically” (The Centre for Psychology + Emotion Regulation, 2024). The patterns of association between eating disorders and substance use vary across these eating disorder types (Root, et al., 2011), with previous studies having found that eating disorders with binge eating/purging behaviors most frequently being associated with higher amounts of substance use (Bahji, et al., 2019). In a study conducted on the patterns of comorbidity of substance use and eating disorders in women in Sweden, substance usage was examined across four eating disorder groups: AN, BN, anorexia nervosa and bulimia nervosa (ANBN), and BED. There was also a control group composed of individuals who did not have an eating disorder. The secondary analyses within the study examined the differences between an AN-R group and AN-B/P group. The results found that, in general, the eating disorder groups had greater amounts of substance usage in comparison to the control group. The AN group in particular had an increased likelihood for usage of all illicit drugs. In the further analysis, the AN-B/P group was found to have a greater “…alcohol/dependence, diet pills, stimulants, and polysubstance use…” than the AN-R group. Across all of the eating disorder groups, the results showed that the BN and ANBN groups reported alcohol abuse/dependency more than the AN group. The ANBN group also had higher reports of diet pill usage in relation to the AN, BN, and BED groups, and the BN group used diet pills more than the AN, BED, and control groups (Root, et al., 2011). Studies on BED have found that one-fourth of individuals with BED have reported substance use disorder, with men with BED reporting higher rates of substance use disorder than their female counterparts (Eskander, Chakrapani, & Ghani, 2020).
Substances of Abuse
The substances associated with eating disorders include alcohol, caffeine, tobacco, illicit drugs, and prescription medications. Alcohol abuse has been found to predominantly affect individuals with eating disorders that contain binging and/or purging patterns of behavior (e.g.: AN-B/P, BN, BED).
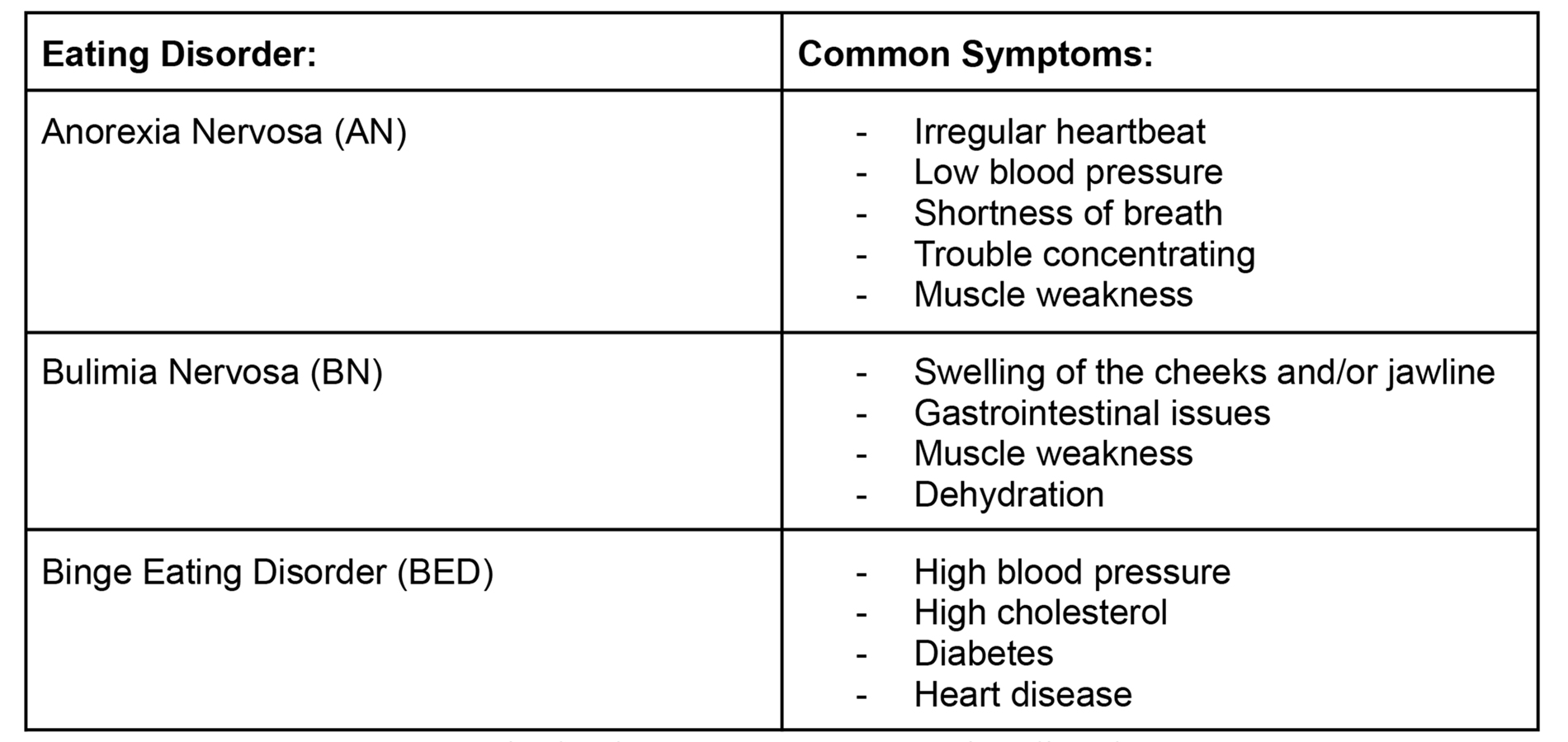
Figure 3. Some substances of abuse atop a scale (Gerke, 2025).
Alcohol use can also be a potential risk factor in “…the development of an eating disorder, [as] studies have indicated an increased prevalence of [eating disorder] behaviours in adolescents using alcohol, with frequency and severity of alcohol consumption found to be positively associated with [many eating disorder] symptoms” (Gregorowski, Seedat, & Jordaan, 2013). Caffeine is used as a source of energy, or as an appetite suppressant. Likewise, tobacco also works as an appetite suppressant, and can also be used to distract from food-related thoughts. Caffeine abuse disorder is associated with distorted body image, and tobacco use is linked “…with greater levels of eating disorder pathology” (Gregorowski, Seedat, & Jordaan, 2013). Illicit drug (including amphetamines, stimulants, cannabis, and opiates) usage is more common within eating disorder populations in comparison to healthy controls. These illicit substances may be used to aid in weight-loss; however, more research is needed in order to clarify the relationship between these illicit substances and the eating disorder subgroups. Of all the substances, laxatives, which fall under the category of prescription medications, are believed to be the most abused substances by individuals with eating disorders, “… [with a] prevalence [rate] of up to 75% being reported in this population” (Gregorowski, Seedat, & Jordaan, 2013). Diet pills are reported far less in comparison to laxatives, and diuretics are primarily used as a purging method for individuals with BN (Gregorowski, Seedat, & Jordaan, 2013).
Figure 4. The laxative selection at a grocery store pharmacy (Gerke, 2025).
Theories
There is no shortage of research demonstrating that a comorbidity between eating disorders and substance use disorders exists, however, there is a lack of definitive answers as to why this relationship exists and what the interaction entails. Although information addressing the underlying nature of this comorbidity would be beneficial for both clinical and research purposes, there has not been enough research into the relationship between eating disorder symptomology and substance use to draw any conclusions (Wolfe & Maisto, 2000). Several hypotheses have been proposed to explain this relationship; for example, alcohol use disorder and eating disorders could be due to a general dysregulation within behavior, such as impulsivity, or a lack of emotional regulation. Binge drinking behaviors could also be attributed to attempts to restrict alcohol consumption (possibly due to the high calorie content), as studies have found “… that restriction of a substance such as food or alcohol leads to increased reinforcement value for that or other substances” (Gregorowski, Seedat, & Jordaan, 2013). In speaking to Kelly Adler, a registered clinical counsellor who has specific expertise in eating disorder and trauma, she echoed the sentiment that the root of this issue stems from “…a dysregulated nervous system and a dissociation, [with an individual] trying not to feel [their] feelings because they feel overwhelmed[, as] both drugs and alcohol and binging, purging, and restricting are all dissociative” (personal communication, February 26, 2025). In general, the theories pertaining to the cause of this relationship tend to fall into two categories: causal etiology and shared etiology. It should be mentioned, however, that none of the following proposed hypotheses have been consistently or sufficiently supported using empirical evidence (Wolfe & Maisto, 2000).
Causal Etiology
Hypotheses based on a causal etiology suggest that by having problems within one area, an individual is at risk for a problem developing within another area. One such hypothesis is the self-medication hypothesis, which suggests that individuals may be using substances to reduce affective symptoms, or to alleviate feelings of anxiety “… resulting from a premorbid anxiety disorder and/or the eating disorder itself”. Another common hypothesis based on causal etiology is the food deprivation hypothesis, which states that by removing a primary reinforcer (in this case, food), an increased value is placed on a different available reinforcer, such as drugs or alcohol (Wolfe & Maisto, 2000).
Shared Etiology
Hypotheses that consider a shared etiology purpose that the relationship between eating disorders and substance use disorders are based upon a predisposition for both disorders. In the personality hypothesis, the idea of an addictive personality style is thought “…to be a common mechanism for vulnerability to a wide range of addictive substances and behaviors”. This hypothesis is based upon the finding that individuals tend to be addicted to more than one substance. For this theory to apply to the comorbidity of eating disorders and substance abuse disorders, two assumptions must be made; firstly, that eating disorders are marked by an addictive behavioral pattern; and secondly, that there are personality traits that exist within these individuals that can be identified as a marker to a predisposition for these two disorder types. Another shared etiology hypothesis proposes that the endogenous opioid system plays a role within the etiology of bulimia, with individuals becoming addicted to the increase in beta-endorphin levels that come from bingeing and purging behaviors. Family history has been hypothesized as a contributing factor to the relationship between eating disorders and substance use disorders, due to the widely accepted notion that a family history of substance abuse tends to be a risk factor in the development of substance use disorders. However, the role of a familial link is unclear within the context of eating disorders (Wolfe & Maisto, 2000).
The Future of This Research
Though there are many studies and analyses on the topic of the comorbidity of eating disorders and substance use disorders, it is clear that there is research to be conducted. As previously stated, there is a lack of understanding as to why this relationship exists, and conflicting findings on the substance use patterns across eating disorder types. It should also be taken into account that a majority of the existing research focuses on the three most common eating disorders (AN, BN, and BED), and primarily conducts their research using female participants. This creates a noticeable gap in the research- what about other eating disorder types, and other genders? During a conversation with Kelly Adler, she stated that a majority of her patient demographic is emerging adults ages 18 to 25, both male and female, noting that “…there’s a real myth that eating disorders only affect young females…they affect all ages and all genders” (personal communication, February 26, 2025). Outside of AN, BN, and BED, Adler also sees “… a lot of orthorexic presentations” as well as avoidant/restrictive food intake disorder (ARFID) (personal communication, February 26, 2025).
Figure 5. Search bar from the EDAnonymous Reddit forum (Gerke, 2025).
Note. Screenshot taken by Gerke (2025) from the forum EDAnonymous hosted on the website
Reddit.
Taking a look at eating disorder forums such as r/EDAnonymous on Reddit, it becomes quite apparent how the eating disorder community at large is affected by substance abuse; one post, for example, reading:
“…most of the time [when I] abuse substances[, it is mostly] just alcohol and a little bit of weed[, and] it is specifically to cope with my failures as far as restricting calories [or to try and] get so messed up [I] just forget what [I’m] dealing with in my weight and abnormal to dangerous eating habits…” (peachy_bicht, 2019).
The forum also contains posts from demographics that were not present in the existing research, such as transgender individuals, as a post titled “I feel like I have to starve because I’m Trans” explains:
“…My recovery body is overweight and I don’t know how to fix it without starving…I look disgusting overweight and it makes me look far more like a man. My ability to accept myself and attempt to pass is life or death” (not_cassy, 2025).
There are also posts discussing a lack of support for less common eating disorders, such as ARFID:
“Whenever I try seeking an [eating disorder] therapist, they always assume I have [anorexia or bulimia], which [kind of] makes me feel like [ARFID] isn’t a “real” [eating disorder]. Whenever I try [to specifically seek out ARFID] support groups, every single other person has autism and I can’t relate to anything in the group besides [ARFID]. I just feel like [ARFID] isn’t talked about enough, especially with non-autistic people” (yeszhongwen, 2024).
Substance use usually begins in adolescence, but substance use disorder prevalence rates peak in early adulthood. Substance use disorder rates are also significantly higher among males, yet there is a stark underrepresentation of male participants in existing eating disorder research, making it so the estimated prevalence does not fully represent all individuals with eating disorders. To better understand the rates of substance use disorder among eating disorder populations, further research needs to be conducted, with more focus on males, as well as children, adolescents, and the elderly (Bahji, et al., 2019).
The Future of Treatment
Along with research methodology, treatment options should be further developed as well. According to Kelly Adler, the primary issue is that “…there’s not really anywhere that [one] can get treated for both [an eating disorder and substance use disorder] at the same time…[which creates] big problems in treatment” (personal communication, February 26th, 2025). When considering a treatment option, both the eating disorder and substance use disorder should be taken into perspective simultaneously, as it is very likely that they are associated (Rittenhouse, 2021), and working “…synergistically, as the development of one disorder appears to be facilitated and/or sustained by the development of the other” (Bahji, et al., 2019). By treating an individual for their eating disorder without also treating their substance use disorder (or vice versa), it heightens the risk for symptom substitution, which occurs when one problematic behavior is replaced with another (Bahji, et al., 2019). To improve the treatment of individuals with a comorbid eating disorder and substance use disorder, eating disorder treatment programs should consider implementing tools to screen for substance use, and treatment programs for substance use disorders should be informed on the signs and treatment methods for eating disorders. By introducing these measures, both disorders can be recognized and treated concurrently (Eskander, Chakrapani, & Ghani, 2020)
Conclusion
Eating disorders are a categorization of mental disorders characterized by a disturbance in eating behaviors. The three most types of eating disorders are anorexia nervosa, bulimia nervosa, and binge eating disorder (Feng, et al., 2023). Substance use disorders are disorders in which an individual has difficulty controlling their use of substances, such as drugs, alcohol, and medications (National Institute of Mental Health, n.d.). It has been found that in their lifetime, approximately one in five individuals with an eating disorder will also develop a substance use disorder, with some studies finding that eating disorders marked by specific behaviors, such as bingeing and purging, have a higher prevalence of substance use disorders (Bahji, et al., 2019). Even though existing research displays a clear comorbidity between these disorders, there is still research to be conducted within the realm of the patterns of association between eating disorder types and substance use disorders. There is also a need for further research into why this relationship exists, as no theory has been consistently supported with empirical evidence. Going forward, the research into this relationship should also consider looking into other populations, as the existing studies tend to use female samples.
References
Bahji, A., Mazhar, M. N., Hudson, C. C., Nadkarni, P., MacNeil, B. A., and Hawken, E. (2019). Prevalence of substance use disorder comorbidity among individuals with eating disorders: A systematic review and meta-analysis. Psychiatry Research, 273, 58-66. https://doi.org/10.1016/j.psychres.2019.01.007
Easton, E. (2023). Anorexia Nervosa Subtypes: Understanding Restricting Type and Binge-Eating/Purging Type. Eating Recovery Center. https://www.eatingrecoverycenter.com/resources/anorexia-subtypes
Eskander, N., Chakrapani, S., & Ghani, M. R. (2020). The Risk of Substance Use Among Adolescents and Adults With Eating Disorders. Cureus, 12(9). https://doi.org/10.7759/cureus.10309
Feng, B., Harms, J., Chen, E., Gao, P., Xu, P., & He, Y. (2023). Current Discoveries and Future Implications of Eating Disorders. International Journal of Environmental Research and Public Health, 20(14). https://doi.org/10.3390/ijerph20146325
Gregorowski, C., Seedat, S., & Jordaan, G. P. (2013). A clinical approach to the assessment and management of co-morbid eating disorders and substance use disorders. BMC Psychiatry, 13, 289. https://doi.org/10.1186/1471-244X-13-289
Hilbert, A. (2023). Psychological and medical treatments for binge-eating disorder: A research update. Physiology & Behavior, 269. https://doi.org/10.1016/j.physbeh.2023.114267
Mayo Clinic. (2024). Anorexia Nervosa. Mayo Clinic. https://www.mayoclinic.org/diseases-conditions/anorexia-nervosa/symptoms-causes/syc-20353591
National Institute of Mental Health. (n.d.) Substance Use and Co-Occurring Mental Disorders. National Institute of Mental Health. https://www.nimh.nih.gov/health/topics/substance-use-and-mental-health
not_cassy. (2025). I feel like I have to starve because I’m trans. [Online forum post]. Reddit. https://www.reddit.com/r/EDAnonymous/comments/1jgu7uh/i_feel_like_i_have_to_starve_because_im_trans/
peachy_bicht. (2019). Is it common for people with disordered eating to also have linked issues with abusing substances occasionally? [Online forum post]. Reddit. https://www.reddit.com/r/EDAnonymous/comments/ccpnsa/is_it_common_for_people_with_disordered_eating_to/
Rittenhouse, M. (2021). Eating Disorders & Substance Use: Co-Occurring Disorders. Eating Disorder Hope. https://www.eatingdisorderhope.com/treatment-for-eating-disorders/co-occurring-dual-diagnosis/alcohol-substance-abuse
Root, T. L., Pisetsky, E. M., Thornton, L., Lichtenstein, P., Pedersen, N. L., & Bulik, C. M. (2010). Patterns of co-morbidity of eating disorders and substance use in Swedish females. Psychological Medicine, 40(1), 105–115. https://doi.org/10.1017/S0033291709005662
The Centre for Psychology + Emotion Regulation. (2024). What is the Difference between Anorexia Nervosa with a Binge/Purge Subtype and Bulimia Nervosa? The Centre for Psychology + Emotion Regulation. https://www.psychology-emotionregulation.ca/uncategorized/what-is-the-difference-between-anorexia-nervosa-with-a-binge-purge-subtype-and-bulimia-nervosa
Wolfe, W. L., & Maisto, S. A. (2000). The relationship between eating disorders and substance use: Moving beyond co-prevalence research. Clinical Psychology Review, 20(5), 617-631. https://doi.org/10.1016/S0272-7358(99)00009-4
yeszhongwen. (2024). I feel like I’m the only person with arfid. [Online forum post]. Reddit. https://www.reddit.com/r/EDAnonymous/comments/1cume1t/i_feel_like_im_the_only_person_with_arfid/
