
Kaeli Seddon
After graduating High School, Kaeli Seddon started attending Capilano University for Classical Music studies. Wanting to synthesize her passion for music with the helping profession, Seddon is pursuing her Bachelor of Arts in Psychology, completing her Associates of Science degree, and is now preparing to apply for Medical School. She advocates for increased accessibility for wellness care.
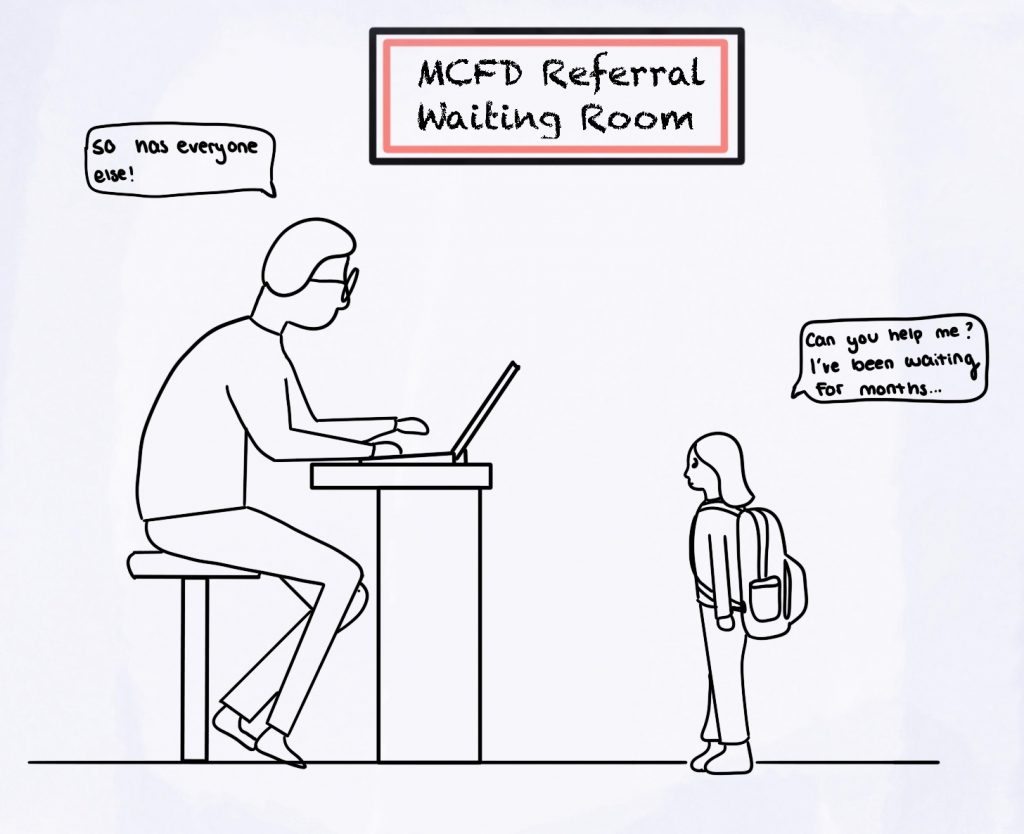
The Canadian Mental Health Association (CMHA)in 2021reportedthat84,000 children and youth in British Columbia were diagnosed with a mental health disorder. Of those 84,000, less than one third received the services they were seeking(CMHA, 2022). These figures reflect only those who have obtained a medical diagnosis, which may not be an accurate reflection of the true numbers of undiagnosed children and youth struggling with their mental health. According to mental health practitioners that I have interviewed, there is a significant disconnect between obtaining support children and youth need, due in part to the Ministry’s method of qualifying for care. Boxes need to be checked, waitlists are long, and even successful candidates that are able to circumvent the government’s requirements are not guaranteed access to professionals trained to cater to that individual’s specific needs(Brady,2022).The system is currently designed in the most expensive way possible, where the most accessible way for our children and youth to obtain care is to reach crisis; this means hospital stays and jail as alternatives to treatment(CMHA, 2022). The government of British Columbia in 2010 estimated that $6.6 billion was spent on mental health problems. In summary, it is difficult for our children and youth to obtain access to resources they need, to receive a diagnosis, and follow through with targeted professional help. The Ministry of Children and Family Development (MCFD)is not consistently providing for those needs, and the current methods in place are expensive alternatives. It is my belief that the triumvir of the three main wellness systems offered to the public by the government of British Columbia; Healthcare, Education, and Family Services would be a powerful combination of public health interventions for our children and youth struggling with mental health disorders. This combination, intertwined with amore holistic approach to wellness, are essential to children and youth to be on the path of mental wellness in British Columbia and everywhere.
The treatment and care for mental illness have come a long way in the last sixty years. Antipsychotic medication was first developed and made in the 1960s to quiet the hallways and to lower staffing requirements in the psych-wards (Dozois, 2019).Candidates for lobotomies were difficult patients with whom nursing staff found not easy to manage. These procedures were performed without consideration to the long-term repercussions of brain tissue removal. The reputation surrounding the topic of mental health, whilst still is stigmatized today, was debilitating to families and individuals that were struggling. While significant improvements have been made since that era, there are still many reoccurring problems and themes that exist today. Selective Serotonin Reuptake Inhibitors (SSRIs), the most common type of prescribed medication to treat many psychological conditions, and Neuroleptics, the psychotropic medication more often referred to as antipsychotics, have had negligent revision in the last sixty years, despite the reformation of our wellness care(Dozois, 2019).For example, it has been demonstrated that participants in Nitzan, et al.’s study(2020) who had diagnoses of Major Depression Disorder (MDD) responded statistically as well to prescribed antidepressants as they did to an open-label placebo options, despite many participants reporting at the end of the study they were aware they had been changed onto a placebo. Another recent example was demonstrated in Schienle and Jurinec’s study (2021),where they found that their participants diagnosed with a mental illness saw the most improvement of symptoms when they were treated with a combination of Cognitive Behavioural Therapy (CBT) and a placebo medication. In addition, there has been discussion in the medical field surrounding the prescription of lithium for people who have Bipolar Disorder (BP) as long-term usage has been demonstrated consistently to cause chronic kidney disease and there are other lower-risk alternatives (Ohlund et al. 2018).
This is why it is a particularly hard pill to swallow–pun not intended—there has not been a serious recall or review of the usage and prescription of such medications to treat mental illness since its inception. In a time where the pharmaceutical industry alongside health care are competing in the same arena as capitalism, medication has accidentally become a top-player. According to the Patient Safety Network, the median rate error of medication rate ranges from8%-25% (2018), and the estimate from the NSDUH Data Review estimates many as 18 million people aged 12 or older have misused prescription psychotherapeutic drugs every year (Jacobson, 2019).This does not take into account the difficulties and problems with obtaining an accurate diagnosis for a mental health disorder in the first place; a poll taken in Kelowna in 2015 reported that 38% of the participants said it took over a year to receive a follow-up from their waitlist status to get a mental health diagnosis (Latimer, 2015), and the feedback from the community demonstrates that things have only gotten worse over time. In Vancouver, the wait-time in July of 2021 for children and youth to be referred to a psychiatrist was 16 months (Gul, & Nassar, 2021).Here in British Columbia, 700,000people in the province do not have a family doctor, and in turn, registered therapists are not covered in standard healthcare(The Times Colonist, 2022). Waiting months or years for help is embarrassing and shameful to what the BC Government calls on their page “accessible healthcare”(Province of British Columbia, 2022).

“The commercial model of health is not healthy.”–M. Fenster, BA (Hons).
My Story I am both academically and emotionally tied to this topic. When I was in middle school, I fought a personal battle every day to get out of bed and go to school. I was being terribly bullied, I had no circle, and my once-stable foundation of my home and family had become inattentive and fragile with my grandmother’s slow decent into her passing. I had a terrible experience getting help; the school counsellor -a woman I had never met before-called me publicly to her office, where she had a pen and notepad scribbling and analyzing any action or inaction I made. Without any trust built, she asked me incredibly intrusive questions, and at the end of it she recommended for me to seek psychiatric care. As an 11-year-old, I had no idea what that meant. Following down that rabbit hole, medical professionals were quick to give me labels as to what was wrong with me, but not one of them asked me about my school or home life. The option of medication was presented to my parents, but I was grateful that they hesitated before accepting that advice, seeking a registered clinical counsellor to visit with me each week first. Had it not been for my parents advocating for me, and them having the financial means to pay out of pocket for them to do so, I would have been receiving treatment for diagnoses ranging from Generalized Anxiety Disorder, Major Depression Disorder, Obsessive-Compulsive Disorder, Dissociative Personality Disorder, and more. I was fortunate that with the help of long-term care and talk therapy, all those diagnoses were tossed aside for a much simpler explanation: Post-Traumatic Stress Disorder. I continued with my talk therapy and specialized care, and now I can confidently say it no longer gets in the way of my every-day life.
A story I am familiar with did not end so well. This person, like me, struggled with mental health as a teenager. Unlike me, their parents nodded along with everything the medical professionals told them. After eight long years of seeking and experimenting with different 6treatments, they were finally diagnosed and treated accurately with Bipolar Disorder. In that time, they had been hospitalized at least four and as many as 15 times a year due to the contraindications of the mixing of medications, the overly high dosages for their age and weight, and this person would suffer enormously from many negative side effects. Doctors would prescribe medication, but without a family doctor or pediatrician, they would not have consultations or follow-ups. The family could not afford counselling services, and because she was not labelled as being in crisis, she was not a candidate to receive help from the MCFD. Her psychiatrist visits were few and far between, and would entail seeing a new doctor every time, none of which were consulting each other about her case. She was one of the 56,000 children each year that slipped through the cracks of the BC government’s ‘solution’ to mental wellness care.
I believe that medication for mental illness, when applied appropriately, can have a significant positive impact on the well-being of an individual. However, my life experience working with children and youth has demonstrated that medication has been overly and sometimes inappropriately prescribed as a solution, financially incentivised for access to more resources, and used in lieu of other less invasive treatments. Children’s neuroplasticity makes them more susceptible and vulnerable to the negative effects of these medications (Hutchison, et al. 2019)and have shown inconsistent results when used for treatment when compared to adults (Amitai et al. 2020). The BC Government’s website clearly states that the first line of treatment is talk therapy (MCFD, 2022), however the definition and application is not made clear anywhere on their website, nor are the educational requirements listed in order to engage in a talk-therapy session with a child or youth. As well, funding for talk-therapy, time for talk-therapy, and follow up for talk-therapy such as when to refer forward are not defined anywhere on their page. As such, well-intentioned adults run the risk of making matters worse for children and youth.
SSRIs is a functional antagonist medication that works to inhibit the reuptake of serotonin(Dozois, 2019). By blocking the ability to reabsorb serotonin, the amount of the neurotransmitter will gradually increase. Because the diagnosis of depression, anxiety, and other mental illness relate to decreased amounts of serotonin, SSRIs are the most commonly prescribed antidepressant medication (Mayo Foundation for Medical Education and Research(MFMER),2019). However, there is a considerable amount of diversity in the individual experience intaking this medication. In Gibson et al.’s qualitative study (2016), out of the1747 participants taking antidepressants, 16% reported having negative experiences, and 28% shared they had mixed experiences. The54% of participants who reported having a positive experience, they shared in open-ended interviews that antidepressants were necessary for their treatment, a way of participating in social and societal obligations, and served as a stepping-stone towards obtaining further help. On the other side, participants reported negative reviews including being ineffective, having a masking effect on real problems, reducing the feelings of control, and unbearable side effects. These side effects can include but are not limited to nausea, headaches, drowsiness, insomnia, dizziness, sexual problems, agitation, and nervousness (MFMER, 2019). Additionally, antidepressants carry black box warnings, as children, youth, and young adults under the age of 25 may experience an increase in suicidal thoughts and behaviours whilst taking them (MFMER, 2019).People working in mental health need to recognize and understand that antidepressants are not to be used as a ‘one size fits all’ solution; care and monitor needs to be a priority when prescribing these medications to children and youth(CMHA, 2022).
“What [we] do understand about the neuroplasticity and the developing brain is how sensitive it is to any and all medications. That can be in a good way, but it can have negative long-term repercussions. […] A question I get asked sometimes is ‘would you put your own kid on medication’;[…First,] I prescribe exercise, sleep hygiene, diet, hydration, and [seek ways to fulfill] the basic human need of being seen.”–G. Brady, RCC.
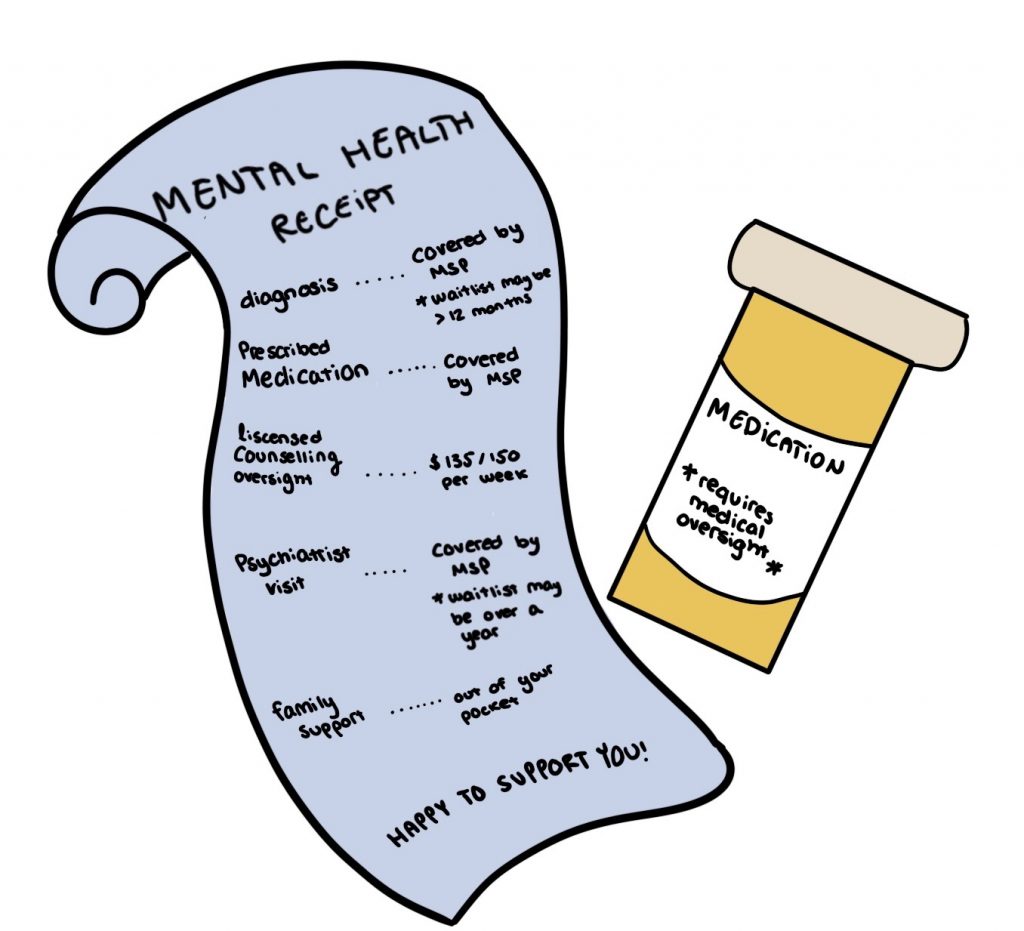
When presented with this information, I am left wondering how it can be ethical to prescribe these medications when children cannot have access to counselling. This may just be an oversight, however, to further elaborate, the BC Medical Services Plan (MSP) covers visits with psychiatrists, but it does not cover counselling services unless you have been referred via a hospital program, police sanctioned, or have been successful in the application and came next on the waitlist through the MCFD(2022). The order of operations simply does not make sense; first you must apply to be on a waitlist for an indefinite amount of time, hope that the application is not rejected, receive an evaluation, and if you receive a diagnosis you can be prescribed medication but may or may not receive funding for additional counselling services, or receive no diagnosis and the train tracks stop therefor government assistance unless you reach a point of crisis. In the defence of the BC government, their page articulates that some extended healthcare plans may claim “up to $500 worth of [counselling] services, per family, per calendar year” and “you must pay for the service cost up-front and submit a claim to the extended healthcare benefits provider for reimbursement, which is subject to plan maximums and reimbursement rate”(Province of British Columbia, 2022). Not only are extended healthcare plans unavailable to many British Columbian citizen, reimbursement plans can still be inhibitory to many families. To add salt to the wound, the average rates of $135-$150per 50-minute session (BCACC, 2021), that would not even fully cover 4 sessions. It does not take an economics specialist to determine that asking an entire family to have to split that annually is an insulting performance of advocacy and availability.
“We shouldn’t have to buy the feeling of health.”–M. Fenster, BA (Hons).
An overhaul and revaluation of what access to wellness care looks like to citizens of BC is required for to secure the health of our future generations. As a person who identifies as a servant to the helping profession, I am extremely passionate about advocating for ways to encourage mental health and seeking alternative for treating mental illness. After spending over 10 years working with children in a variety of capacities, ranging from education, afterschool programs, and summer camps, I have been both privileged and honoured to have been entrusted to stories of children struggling with their mental illness diagnosis, the medications they have been inconsistently prescribed, and the cries for help for seeking something different.
The first change to be considered includes a “marrying” of the three triumvirs of wellness support: The Ministry of Health, the Ministry of Education, and the Ministry of Children and Family Development in order to provide a more bulletproof model of holistic care. This model is currently under testing in many communities in British Columbia. Second, increase the accessibility to counselling resources based on interventions from the medical community with support from education and the MCFD. Third, a system of follow-up care and support needs to be in place with regular standard procedures in place for mental health and wellness. This describes a universal healthcare model that includes mental wellness and support. As the stigma surrounding mental health evolves in its compassion, understanding, and recovery, wellness services then become included as a standard part of our standard inclusive healthcare system.
When children and youth first reach out, the first step should be to immediately have the child at risk and their family connect to a registered clinical counsellor to seek professional consult and care. This professional should be able to see them through any waitlist to seek higher-level medical care or evaluation. In many cases, talk-therapy with a trained and licensed trauma-informed therapist may be all that is required. If further interventions are needed, having this connection can be vital in the prevention of reaching crisis.

Additionally, there needs to be the opportunity for children and youth to explore a variety of options as alternatives to medication for their treatment. Options such as Music Therapy, Guided Imagery Meditation, Art Therapy, Eye Movement Desensitization and Reprocessing, Dialectical Behaviour Therapy, Play Therapy, and others have accredited and licensed professionals offering these varying specialties. There is a barrier to public access from exploring these alternatives yet there are evidence-based research and practices coming out of these fields, and thousands of cases of anecdotal evidence from many individuals. I fully believe that if there is a chemical imbalance or irregularity within one’s brain occurring, medication may be the only way to resolve it. However, I believe it is negligent that so many individuals are not able to explore all the other options that are out there because it is not backed up by the BC government.
Finally, I propose that all professionals working with children should be required to receive training that is specific and catered to being able to determine when a child is in need of professional counselling. There have been several instances displayed on news outlets calling out educators working in schools for overstepping their professional boundaries into counselling(Holliday, 2022). These well-meaning professionals are giving advice and counsel from an untrained perspective may cause even more harm to the children seeking care in the first place. Professional development that educates working professionals on what counselling and therapy is, how to determine if a child is in need, practice as to how to make a report to MCFD, and how to connect these children to trained and accessible resources needs to be mandated by the BC government, and needs to be a requirement in order to continue working in these settings. In my bold opinion, any professionals and para-professionals working with children, youth, and families must be trained in trauma-informed practice.
Radical changes are required to the processes involved with children and youth receiving a diagnosis and care. Children should not have to wait two years on a waitlist to receive help they require: instead, we the professional caregivers should be asking what is the maximum amount of time we can ethically leave a child or youth on a waitlist for mental health support? Children should not have to be in crisis, using resources such as law enforcement and hospital beds as the only way to get the attention they demand. And it is my belief that children should not be prescribed medication unless they are under the care and monitor if a licensed clinical counsellor or psychiatrist. Doctors, educators, and people who work directly with children should not only be advocating for changes but should be required and provided training on trauma-informed practice. The same way it would not make sense to put a band-aid on without first cleaning the wound, an investment needs to be made towards taking care of the individuals impacted by mental illness before we give them a label and a prescription. Medication alone is not a solution to mental illness, and there is no ethical way to hand out mental wellness medications without the care of medical professionals overseeing the usage.
Works Cited
Amitai, M., Taler, M., Lebow, M., Ben-Baruch, R., Apter, A., Fennig, S., Weizman, A., & Chen, A. (2020). An increase in IL-6 levels at 6-month follow-up visit is associated with SSRI-emergent suicidality in high-risk children and adolescents treated with fluoxetine. European Neuropsychopharmacology, 40, 61–69. https://doi.org/10.1016/j.euroneuro.2020.07.007
Brady, G. RCC., Personal Communication, March 30, 2022.
Dozois, D. J. A. (2019). Abnormal Psychology Perspectives(6th ed.). Pearson.
Editorial: These factors have brought family-doctor system to brink of collapse. The Times Colonist. (2022, February 11). Retrieved April 8, 2022, from https://www.timescolonist.com/opinion/editorial-these-factors-have-brought-family-doctor-system-to-brink-of-collapse-5052487#:~:text=Throughout%20B.C.%2C%20about%20700%2C000%20people%20do%20not%20have%20a%20family%20doctor.
Fenster, M., BA (Hons)., Personal Communication, March 31, 2022.
Gibson, K., Cartwright, C., & Read, J. (2016). ‘in my life antidepressants have been…’: A qualitative analysis of users’ diverse experiences with antidepressants. BMC Psychiatry, 16(1). https://doi.org/10.1186/s12888-016-0844-3
Government Communications and Public Engagement. (2022, March 11). Health. Province of British Columbia. Retrieved April 8, 2022, from https://www2.gov.bc.ca/gov/content/health#:~:text=B.C’s%20publicly%2Dfunded%20health,services%20through%20the%20PharmaCare%20program.
Gul, M., & Nassar, H. M. (2021, July 21). Issues with B.C.’s mental health system highlighted by 16-month wait for consultation. CityNews. Retrieved February 25, 2022, from https://vancouver.citynews.ca/2021/07/23/bc-mental-health-waits-system/
Holliday, I. (2022, March 19). Surrey teacher’s counselling of students overstepped ‘professional boundaries,’ Discipline Authority says. British Columbia. Retrieved April 10, 2022, from https://bc.ctvnews.ca/surrey-teacher-s-counselling-of-students-overstepped-professional-boundaries-discipline-authority-says-1.5825905
Hutchison, S. M., Mâsse, L. C., Brain, U., & Oberlander, T. F. (2019). A 6-year longitudinal study: Are maternal depressive symptoms and selective serotonin reuptake inhibitor (SSRI) antidepressant treatment during pregnancy associated with everyday measures of executive function in young children? Early Human Development, 128, 21–26. https://doi.org/10.1016/j.earlhumdev.2018.10.009
Jacobson, A. (2022, January 20). Medication errors statistics. The Checkup. Retrieved April 8, 2022, from https://www.singlecare.com/blog/news/medication-errors-statistics/#medication-errors-stats-by-drug-type
Latimer, P. (2015, August 30). Mental health system study. Kelowna Capital News. Retrieved April 8, 2022, from https://www.kelownacapnews.com/news/mental-health-system-study/
Mayo Foundation for Medical Education and Research. (2019, September 17). The most commonly prescribed type of antidepressant. Mayo Clinic. Retrieved April 10, 2022, from https://www.mayoclinic.org/diseases-conditions/depression/in-depth/ssris/art-20044825
Ministry of Child and Family Development. (2020, July 9). Foster care payments in BC. Province of British Columbia. Retrieved April 8, 2022, from https://www2.gov.bc.ca/gov/content/family-social-supports/fostering/for-current-foster-parents/foster-care-payment
Ministry of Child and Family Development.(2022, April 7). Child & Youth Mental Health Intake Clinics. Province of British Columbia. Retrieved April 10, 2022, from https://www2.gov.bc.ca/gov/content/health/managing-your-health/mental-health-substance-use/child-teen-mental-health/mental-health-intake-clinics
Ministry of Child and Family Development. (2022, March 10). Child & Youth Mental Health. Province of British Columbia. Retrieved April 8, 2022, from https://www2.gov.bc.ca/gov/content/health/managing-your-health/mental-health-substance-use/child-teen-mental-health
Nitzan, U., Carmeli, G., Chalamish, Y., Braw, Y., Kirsch, I., Shefet, D., Krieger, I., Mendlovic, S., Bloch, Y., & Lichtenberg, P. (2020). Open-label Placebo for the treatment of Unipolar Depression: Results from a randomized controlled trial. Journal of Affective Disorders, 276, 707–710. https://doi.org/10.1016/j.jad.2020.07.077
Province of British Columbia. (2022, January 21). Short-term counselling. Province of British Columbia. Retrieved April 10, 2022, from https://www2.gov.bc.ca/gov/content/careers-myhr/all-employees/safety-health-well-being/health/efas/short-term-counselling
Schienle, A., & Jurinec, N. (2021). Combined cognitive-behavioral therapy and placebo treatment for patients with depression: A follow-up assessment. Psychology Research and Behavior Management, Volume 14, 233–238. https://doi.org/10.2147/prbm.s294940
Take action. CMHA British Columbia. (n.d.). Retrieved April 10, 2022, from https://cmha.bc.ca/impact/facts-and-figures/#:~:text=About%2017%25%20of%20British%20Columbians,are%20receiving%20mental%20health%20services.
Vejzovic, V., Carlson, L., Löfgren, L., & Bramhagen, A.-C. (2022). Early identification of mental illness in primary school pupils by School Nurses: A qualitative study. SAGE Open Nursing, 8, 237796082210814. https://doi.org/10.1177/23779608221081452
What does counselling cost? BCACC. (2021, October 22). Retrieved April 10, 2022, from https://bcacc.ca/find-a-counsellor/fee-schedule/
Öhlund, L., Ott, M., Oja, S., Bergqvist, M., Lundqvist, R., Sandlund, M., Salander Renberg, E., & Werneke, U. (2018). Reasons for lithium discontinuation in men and women with bipolar disorder: A retrospective cohort study. BMC Psychiatry, 18(1). https://doi.org/10.1186/s12888-018-1622-1
