
Brittany Oake
Brittany Oake is currently completing her Bachelor of Arts with a Major in Psychology. She has achieved exceptional grades and feedback in her Current Issues in Neuropsychology course which has inspired her to follow a career path in the field of psychedelic therapy.

In 1934 a man named Bill Wilson participated in an experiment where they were investigating the treatment of substance use disorder with an admixture of henbane and belladonna plants that have tropane alkaloids which are deliriants that fall under the classification of hallucinogenic substances (Yaden et al., 2021). Bill went into this experiment with hopes of recovering from his alcohol use disorder, coming to find that a psychedelic trip was his salvation (Yaden et al., 2021). The world drug report in 2019 reported that roughly 35 million people suffer from substance use disorder (United Nations, 2019). What would it look like if we could offer the same treatment that healed Bill to the 35 million individuals who are suffering from substance use disorder?
Many of us have heard of rehab, treatment centers, sobering centers, alcoholic anonymous, the twelve-step program, and other options currently being offered for those suffering from substance use disorder. How often do you hear about recovery through psychedelics? You may have heard whispers or murmurs on the matter, and some may think it is some new age lies, or some may be confused with treating substance use disorder with another substance. This article will take you through the astonishing ability that psychedelics have in a therapeutic setting specifically within addictions. Starting with a current look into our treatment centers today, moving into an influential stakeholder’s beliefs on the connection between trauma and addiction, followed by the research on psychedelics’ abilities to treat substance use disorder. By the end of this article, you may find yourself asking the question of why we are not utilizing psychedelics in our British Columbia Mental Health and Substance Use Services.

In an interview with Alex Patterson, who is a program assistant in a local treatment center, she was asked if she felt the clients at her centre utilized the counsellors on-site and what her opinion was on their impact on the client’s recovery.
“I think it’s an essential piece, to be honest. There are certain floors that only have one counsellor and other floors that have two and you can see the direct difference between the two floors… floors that have two counsellors-there is more engagement… overall interaction with somebody that cares and is there five days a week consistently… I mean I really don’t think the programming would work if there weren’t counsellors on each floor.”
Asking her if there was a negative component she could touch on, “at times there can be too many residents to truly get to the root of these individuals’ problems”. Alex was able to highlight that her treatment center is quite structured, they have a larger emphasis on giving people the skills and tools needed to create a more balanced daily life. Having group therapy and daily available counsellors that can check in with their clients and make sure that they are handling their recovery and treatment- not necessarily there to heal past traumas. These parts are key to recovery for many individuals as another interviewee Dr. Gordon discusses, there are, “two parts to recovery, structural and psychological.”
Getting the chance to interview Dr. Gordon who has a vast knowledge and understanding of this field, with her background being in experimental neuropsychology. Dr. Gordon was able to answer questions from a more clinical perspective. Asking her if she felt there was a point in a person’s recovery when it is too late to go back and mend past traumas that could be the root of some individual’s substance use. From a structural point she believes that a person needs to support themselves, house themselves, and feed themselves before you can start to delve into the psychological aspects of their addiction- “…Once you have the cognitive functions to control emotions and behaviours, you can then start looking at how to heal the trauma that brought them to their substance use disorder.”

Taking the chance to discuss with Dr. Gordon what her thoughts were on other forms of therapy. More specifically, if she believed that if we had psychedelic therapies as an option within our treatment centers would the clients engage and utilize them? She rephrased it and said, “The minute it becomes a service in its true form- service as in you aren’t forcing people into rehab… it’s not court-mandated… and how can we help you, you are the client…yeah believe me engagement happens.” This was an insight into the power of intent of service, and how that affects client engagement. Talking to Alex and Dr. Gordon was a good introduction to what our current system looks like, and what we are focusing on. It seems that we are offering the structure that many individuals seek when going through their recovery, but we may be missing a key element when it comes to the psychological aspect of serving them.
Dr. Gabe Maté as Dr. Gordon described is a pioneer in addictions in the Vancouver Downtown East Side, “He was one of the first to get in there and say we need to change our practices.” She gives credit to Dr. Gabe Maté for being the one who sought insight into hallucinogenic assisted therapies within our city.
“Here on the Downtown Eastside, he was doing the research with ayahuasca and insight in psychotherapy…in its two fronts, the first idea is the kinds of therapies and how do you from a psychotherapeutic approach deal with individuals who have addictions, what are you targeting? The addiction or the trauma and then there was the second aspect on the institutional level, what are the practices and how do we put them into play.”
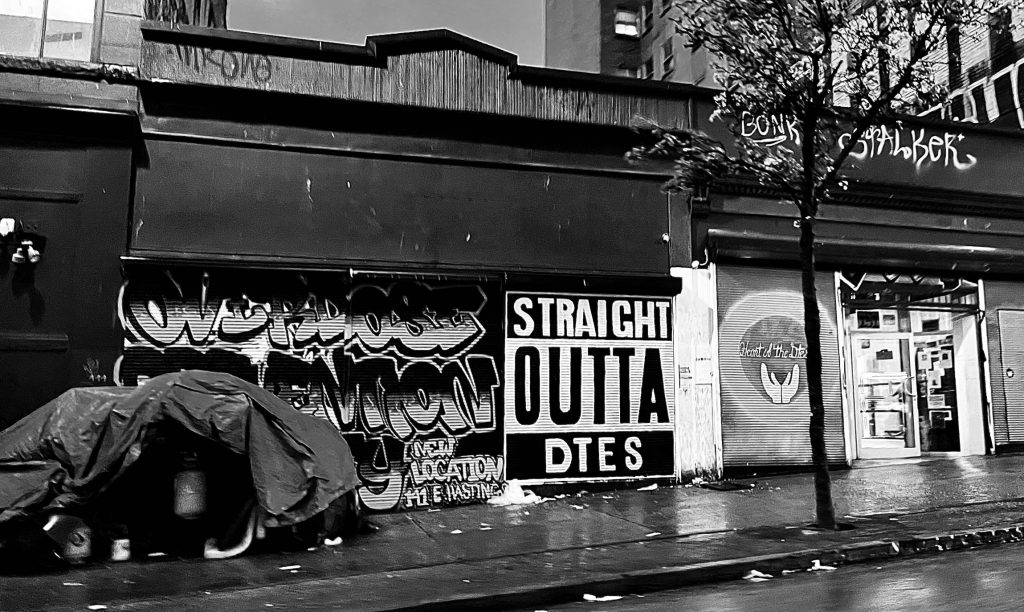
Dr. Gabe Maté (Waters, 2019) talks about how our Downtown Eastside is one of North America’s most intense areas of drug use. In Dr. Gabe Maté’s twelve years of working within the Downtown Eastside, he can contest that the hundreds of female patients he worked with had experienced sexual abuse as children. His male clients reported being sexually, physically, and emotionally abused. They had been neglected and were at some point in their lives part of the foster care system. Dr. Gabe Maté’s work allows the recognition of how rooted trauma is in addiction, and how necessary it is to find ways to treat these adversities. As Dr. Gabe Maté defines; “All addictions — alcohol or drugs, sex addiction or internet addiction, gambling or shopping — are attempts to regulate our internal emotional states because we’re not comfortable, and the discomfort originates in childhood.”(Waters, 2019). Dr. Gabe Maté found there to be no separation in the addictions he mentions outside of their degree, all addictions affect the same brain circuits, same emotional confounds, and the same pain and outcome of behaviours. The way he explains addiction should open our empathy and shift our stigma. Would you treat a heroin addict the same way as a gambling addict?

To understand how our system within addictions, treatment, and recovery works, we should look to understand the individuals and what has brought them to this point. Our medical system as he puts it is still lacking the training and awareness of practitioners to this knowledge and leaves a large gap between understanding the pain and human suffering these individuals have. He explains that physicians are not at the point where they are being taught to acknowledge the neurobiology of addiction in substances as well as non-substance addictions. We are missing the scientific understanding of how early life experiences affect these aspects and it seems to yet be a valued theory in our medical practice (Koeverden, 2018). Dr. Gabe Maté can be quoted on what our system should look like when we are looking to treatment, “Inclusion, not ostracizing, need to motivate our policies; not punishment but support, not judgment but empathy.”(Means to treating trauma, 2017).
When looking at treatment for substance use disorder it is more complex than what we as a health system have given it credit for. In a literature review done by Catherine et al (2021) they show the effectiveness of psilocybin and 3,4 Methylenedioxymethamphetamine (MDMA) in the treatment of trauma-related psychopathology. Covering the history, practice, and benefits that both psilocybin and MDMA can have in the treatment of post-traumatic stress disorder, major depressive disorder, and treatment-resistant disorder. When looking at a person’s reaction to a traumatic event they typically show symptoms of low mood, anxiety, exhaustion, dissociation, heightened physical arousal, agitation, and numbness (Catherine et al., 2021). Trauma exposure has been connected to multiple psychiatric conditions, including major depressive disorder, dysthymia, bipolar disorder, anxiety disorder, and substance use disorder (Catherine et al., 2021). This study gives an understanding of the mechanisms that are in play when considering trauma and substance use disorder, and how an individual would feel compelled to search for a remedy for these maladaptive symptoms.
Hallucinogenic substances hold the ability to give individuals a sense of harmony, sanctity, indescribable, transcendence of time and space, and a deeply felt positive mood (Yaden et al., 2021). These benefits have been linked to improving individuals’ well-being and reducing anxiety, depression, and substance use disorders (Yaden et al., 2021). The science behind these substances shows that classic psychedelics act on our serotonin system as agonists to the serotonin 2A (5-HT2A) receptors (Yaden et al., 2021). This group of “classic” psychedelics includes psilocybin which is the active chemical in what we know as magic mushrooms, LSD, dimethyltryptamine (DMT), and what some of us may have heard of before- ayahuasca (which includes a mixture of DMT) (Yaden et al., 2021). As with any substance including over-the-counter medications, there are adverse effects that should be noted. When considering hallucinogenic substances their effects are quite mild such as high blood pressure and heart rate with low abuse potential (Yaden et al., 2021). When being used recreationally a person may experience cardiac effects, a destabilization in individuals who may have an underlying predisposition to psychotic disorders, higher levels of anxiety, or dangerous behaviours. All these possible outcomes are highly mitigated when they are being utilized in a clinical setting (Yaden et al.,2021).
In 1934 a man named “Bill” was in New York when he decided to try and seek treatment once again for his alcohol use disorder as his previous efforts had been unsuccessful (Yaden et al., 2021). He entered an experimental treatment at a local hospital that was using an admixture of henbane and belladonna plants that had tropane alkaloids, which are deliriants that fall under the classification of hallucinogens. Bill experienced a bright white light, matched with a feeling of great peace while he was under the influence of the hallucinogenic admixture. He described it as a spiritual, self-transcendent experience. This experience led Bill to never touch alcohol again (Yaden et al.,2021).
Bill had a conversation with a friend of his before this experiment where his friend was raving about how salvation could save him from his alcohol use disorder (Yaden et al., 2021). Because of this conversation, Bill attributed “the bright white light, spiritual, self-transcendent” moment to a spiritual awakening- in his mind finding salvation (Yaden et al., 2021). This experience led Bill to find Alcoholics Anonymous, which included the twelve-step program that many of us are familiar with (Yaden et al., 2021). Bill’s goal with this program was to help others heal and give them a spiritual awakening like the one he had. Bill had taken LSD multiple times after the experiment in New York and felt that psychedelics could be used to aid others in having a transcendent, spiritual awakening he had himself (Yaden et al., 2021). The man who founded Alcoholics Anonymous was inspired by and treated by a hallucinogenic experience and believed that these drugs could be used to heal other’s substance use disorders… in 1934 (Yaden et al., 2021). The board of Alcoholics Anonymous did not let Bill include the psychedelic aspect in the handbook he wrote. They felt it was too confusing of a message, so they hijacked science and replaced it with an emphasis on religion (Yaden et al., 2021). We are almost a hundred years away from that and we are still not utilizing them as a tool in the treatment of substance use disorder.
A case study was done by Johnson & Black (2020) that gives a more personal look at how impactful and beneficial psychedelics can be. The case study was on a man named John. John was enrolled in individual therapy where he was given the diagnosis of major depressive disorder, stimulant use disorder, and cannabis use. Johns’ substance use history was quite extensive but had reported benefiting from the use of classical psychedelics which he was using recreationally and outside of a clinical setting. John stated that during the time of his psychedelic use he had found that his cravings for stimulant drugs had been minimized. It was an experience on psychedelics that John describes as difficult but insightful that he was able to recognize his substance abuse issues. This experience for John is what led him to seek out psychotherapy for the first time. John found that the psychedelics allowed him to see more clearly and made him question his use of stimulant drugs and what they were giving him, as he said stimulants, “Took everything and (left) nothing.” These experiences on classic psychedelics allowed him to self-reflect from a neutral place of observation, giving him the ability to delve deep into his introspection which created his behavioural change and allowed him to heal (Johnson & Black, 2020).

In Catherine et al. (2021) article they were able to feature what undergoing treatment with the use of psilocybin and MDMA in psychotherapy looks like. These substances are used to aid in a positive psychological change by creating a safe, comfortable, trusting, and non-judgmental setting with a supportive therapist present. Clients who utilize this form of treatment would find themselves in a comfortable, quiet, neutrally furnished room, with relaxing music. Typically, the individual going through this process will undergo a preparation session before, and then an integration session after completing the substance-dosing session. It is important that the client can have an inner focus in both forms of treatment. When specifically utilizing psilocybin, it is encouraged to have attention to the internal processes of the individual. This is because the therapist will want to have a discussion after on what was felt, realized, and recognized throughout the dose session (Catherine et al., 2021).
The history of using these substances as treatment goes back quite far. From 1950-to 1970 more than 1000 clinical papers were written on the use of psychedelics as treatment (Catherine et al., 2021). Unfortunately, they were shut down by the Controlled Substance Act (CSA) in 1970, with re-emergence in 1992 (Catherine et al., 2021). In an article written by Ponieman (2022), it states that an amendment to federal regulations, Health Canada has announced they are allowing physicians to request access to drugs like psilocybin and MDMA on behalf of their patients through the Special Access Program. Currently, psychedelic treatment can be sourced and utilized in either a private sector or through an experimental capacity.
Within Vancouver, one of the places you can go to is Gaia Counselling, a psychotherapy service. It is located in Gastown, only blocks from our Downtown Eastside. Some of the substances they use include Psilocybin, LSD, DMT, Ayahuasca, MDMD, and Ketamine. They discuss the different types of themes that can be explored within their psychedelic integration therapy. Here are some of the ones that connect to what we are talking about here today: The importance of seeking the help of a professional therapist to make major life changes that your journey guided you to make. Better processing of difficult or upsetting occurrences. Integration of insights and wisdom gained from your experience, into your daily life. Finally, learning how to process trauma and how to journey back into the body. (Gaia Counselling, 2022). Their utilization and themes do not directly touch on substance use disorder, but they give an even larger insight into the multitude of benefits psychedelics treatment can have outside of this article’s focus.
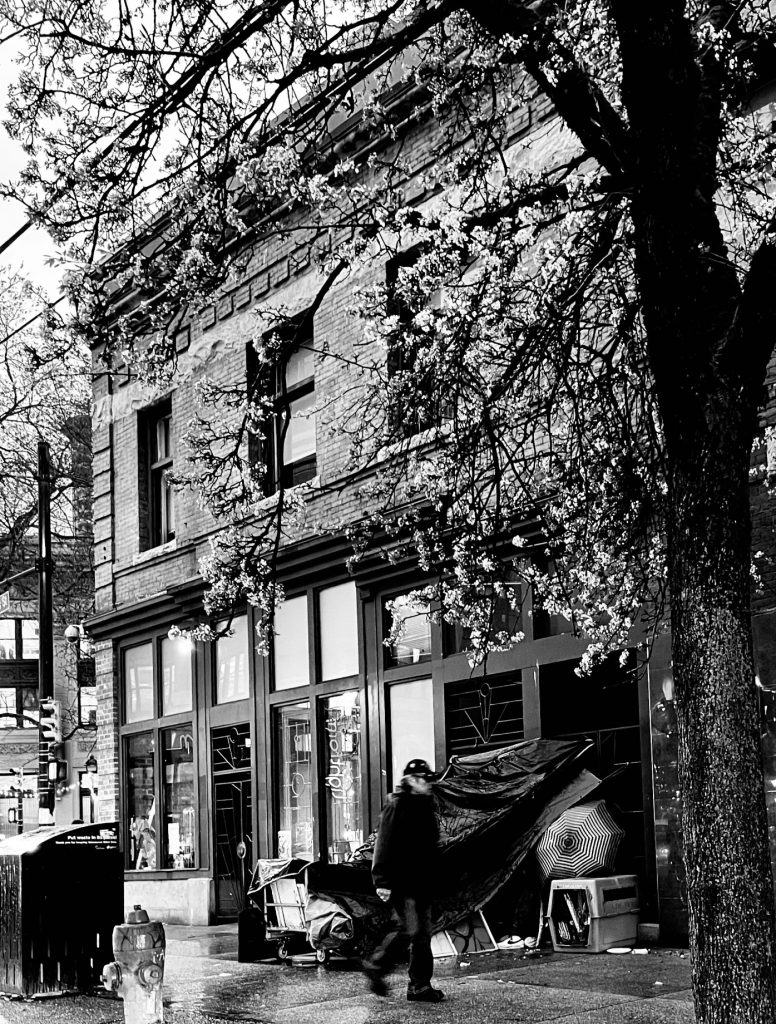
For many years Vancouver’s Downtown Eastside has been impacted by the result of many individuals who suffer from substance use disorder. The results of drug use in our city have been defined by the word epidemic. Substance use disorder affects many individuals right here in our city and province. The streets and alleys in our Downtown Eastside reflect these individuals’ struggles, with one turn down an alley, an abundance of drug paraphernalia can be found. It is difficult to see this and not wonder how we could change our approach to aiding this community. The British Columbia Mental Health and Substance Use Service (BCMHUSUS) put an update out for their directional plan in February 2022. With recent funding from Telus, they are discussing a new launch into viral innovative technologies to aid in the care of their clients (BCMHSUS, 2022). They are looking to keep to their commitment to promoting knowledge translation and exchange through learning rounds in their treatment and care facilities to try and fill the gaps (BCMHSUS, 2022). With keeping their focus on the continuation of innovation, cultural safety, family and person-centred practices while empowering their teams to feel supported and energized to tackle these challenges (BCMHSUS, 2022).

As Dr. Gordon said- when we switch from the force in treatment and recovery and switch to what the individual needs, we will start to see engagement. There is a desire to fix and fill the gaps we have within our treatment system. It could be the perfect time to consider utilizing psychedelics in our public health system in consideration of treatment options. As they mention they are looking for new innovative ways and looking to gain inspiration and new ideas for improving care (BCMHSUS, 2022). Psychedelic treatment may not be a new idea, but it would be innovative and inspiring.
There is a need for more options within our public health system for the treatment of substance use disorder. Even though there are places utilizing psychedelic treatment within our province they are not easily accessible. Moving these options from private to public access could give greater accessibility and more options for individuals that are seeking help and have found our current system isn’t working for them. A place to start could be creating public accessibility to psychedelic treatment. Creating more rigorous studies and experiments within our province utilizing the individuals who are seeking other methods of treatment and see what it could bring to the table, and what this change could look like. Through ninety years of research in the field of psychedelics, they have proven their abilities in treating substance use disorder.
The hope for this article was to give a look into the benefits of psychedelic treatment and what utilizing this tool within our public care system could look like. A tool for the individuals that suffer through their substance use disorder, the ones who try to go to treatment, try to recover but at times find themselves in a vicious cycle. The ones who need help overcoming their past traumas so they can escape the adversities that come with it. Our system works for some, but it doesn’t work for all. Just like any other facet of life, we should have options that focus on the individual, and in this case, individual healing. What implementing classic psychedelics as a resource within our treatment centers and recovery options could do for certain individuals is paramount. It could allow many the chance to heal in a new way, and as John put it find independence in their journey of recovery (Johnson & Black, 2020).
References
Bird, C. I. V., Modlin, N. L., & Rucker, J. J. H. (2021). Psilocybin and MDMA for the treatment of trauma-related psychopathology. International Review of Psychiatry, 33(3), 229–249. https://doi-org.ezproxy.capilanou.ca/10.1080/09540261.2021.1919062
Johnson, S., & Black, Q. C. (2022). Classic psychedelics as a psychotherapeutic aid in the treatment of stimulant use disorder: a case report. International Journal of Mental Health & Addiction, 20(2), 744–753. https://doi-org.ezproxy.capilanou.ca/10.1007/s11469-020-00398-7
Yaden, D. B., Berghella, A. P., Regier, P. S., Garcia-Romeu, A., Johnson, M. W., & Hendricks, P. S. (2021). Classic psychedelics in the treatment of substance use disorder: Potential synergies with twelve-step programs. International Journal of Drug Policy, 98. https://doi-org.ezproxy.capilanou.ca/10.1016/j.drugpo.2021.103380
Gaia Counselling: https://gaiacounselling.com/services/psychedelic-integration/
United Nations Drug World Report 2019: https://www.unodc.org/unodc/en/frontpage/2019/June/world-drug-report-2019_-35-million-people-worldwide-suffer-from-drug-use-disorders-while-only-1-in-7-people-receive-treatment.html?ref=fs1
Ponieman, N. (n.d.). Breaking: Canada opens new legal pathways for access to psychedelics treatment with psilocybin and MDMA. Benzinga. Retrieved May 1, 2022, from https://www.benzinga.com/markets/cannabis/22/01/24913445/breaking-canada-opens-new-legal-pathways-for-access-to-psychedelics-treatment-with-psilocybin-an
Dr. Gabe Maté CBC- Addiction Requires Both Science & Compassion 2018:
https://www.cbc.ca/books/treating-addiction-requires-both-science-and-compassion-says-dr-gabor-maté-1.4792095
Dr. Gabe Maté CBC- Fixing Fentanyl Means Treating Trauma 2017:
https://www.cbc.ca/news/canada/british-columbia/fixing-fentanyl-means-treating-trauma-that-creates-addicts-1.3966361
British Columbia Mental Health and Substance Use Services- Share Vision For the Future 2022: http://www.bcmhsus.ca/about/news-stories/stories/leaders-share-vision-for-future-bcmhsus